Crime
MA/RI Physician sentenced in health care, pain med scheme

BOSTON – A Massachusetts pain management physician was sentenced Thursday in federal court in Boston in connection with his scheme to defraud Medicare and other health care insurers, and then using the proceeds of his illegal activity to support his extravagant lifestyle.
Fathallah Mashali, 62, was sentenced by U.S. District Court Senior Judge Rya W. Zobel to eight years in prison, three years of supervised release and ordered to pay restitution of $8,725,120. In March 2017, Mashali pleaded guilty to 27 counts of health care fraud, one count of conspiracy to commit mail fraud, and 16 counts of money laundering.
Mashali, a licensed physician in Massachusetts and Rhode Island, operated New England Wellness & Pain Management, P.C., a/k/a New England Pain Associates, P.C., of Massachusetts and Rhode Island, a/k/a Greystone Pain Management, Inc., a/k/a New England Pain Institute, P.C. (NEPA). He also employed Egyptian doctors in Cairo, Egypt, who entered false information into U.S. patients’ medical records. Many of the patients at NEPA were Medicare beneficiaries.
From approximately October 2010 through March 2013, Mashali falsely billed Medicare for extensive medical services that he did not provide. He treated patients with chronic pain conditions and frequently gave his patients large doses of prescription medications, including powerful opiates. Mashali falsely stated in patients’ medical records and representations to Medicare and private insurance companies that he had seen patients for 25 minutes per appointment or longer, when in fact, Mashali often saw his patients for less than five minutes. In his brief interactions with his patients, Mashali did not perform any physical examinations and barely inquired into the patient’s medical status or history. In addition, he overbooked his patient appointments and arrived to work sometimes as late as four hours after his first scheduled appointment. His scheduling practices caused significant overcrowding at his offices and left him with no meaningful ability to assess each individual patient. Mashali then falsely documented that he conducted extensive physical exams, when he most often did not even touch his patients. As a result of his false statements, he obtained substantial reimbursement from Medicare and private insurance companies.
“Dr. Mashali ran his pain management practice as a pill mill,” said United States Attorney Andrew E. Lelling. “He overprescribed powerful narcotics without any discernible medical services to patients, and some patients died from overdoses. At one point, Dr. Mashali was one of the highest-volume prescribers of oxycodone in Massachusetts, second only to a leading Boston hospital. He took advantage of patients, his staff and the American healthcare system by defrauding Medicare. This sentence ensures that Dr. Mashali will never again treat – or mistreat – patients in order to line his own pockets at the expense of patient care.”
“Through his fraudulent schemes, Dr. Mashali exposed his patients to unnecessary risks, over-prescribed medications including powerful opiates, and recklessly failed to provide the appropriate level of treatment expected from our health care professionals,” said Harold Shaw, Special Agent in Charge of the Federal Bureau of Investigation, Boston Field Division. “Not only did he exploit Medicare and taxpayer funded programs to support his lavish lifestyle, he lied, cheated, and stole from these programs. Playing fast and loose with the rules undermines the integrity of our healthcare system, contributes to its rising cost, and ultimately impacts on the quality of care expected from health care providers. This case should serve as a warning to others that the FBI is deeply committed to investigating cases of graft and greed in order to protect important taxpayer funded programs.”
Mashali also routinely billed Medicare and private insurers for urine drug test results that were false and fraudulent. He caused patients’ urine samples to be stored for weeks and up to three months unrefrigerated in a sunlit space in his laboratory in Holbrook, Mass., which left them degraded and worthless. The decomposition caused a significant stench of stale urine throughout the lab. Mashali nevertheless made his lab technicians test all the old urine, while well aware that his practice of urine sample storage was wrong. When inspectors showed up at his lab, he directed his staff to move the unrefrigerated urine out of sight.
Mashali mandated that his staff run every patients’ urine sample on two machines, each of which used the same scientific testing methodology, which Mashali knew was contrary to Medicare billing rules. He caused every patients’ urine specimen to be chemically confirmed, despite the fact that he did not even know the result of the initial urine drug screening test, knowing that this was also contrary to Medicare billing rules. Moreover, Mashali ran tests on chemical analyzers that had not been properly calibrated and validated.
When Medicare began to inquire about Mashali’s unlawful billing practices and initiated an audit of Mashali’s medical services, requesting 40 patient medical files, Mashali caused his staff both in the United States and in Egypt to falsely alter patient records. This included falsifying patient encounters which had taken place sometimes one or more years earlier, and faking and backdating the results of patients’ urine drug tests. Mashali knew that his patient records would not pass muster with Medicare’s auditors and thus ordered his staff to make these changes.
Mashali used the proceeds derived from his fraudulent billing to fund a lavish lifestyle, spending money on his extravagant Dover residence and a condominium in Florida. For example, he ordered the construction of a carriage house and outfitted his Dover home with a squash court and movie theater.
“Today’s sentence underscores our ongoing commitment to protecting the American people from all forms of healthcare fraud, safeguarding taxpayer resources and ensuring the integrity of essential healthcare programs,” said Special Agent in Charge Phillip M. Coyne of the U.S. Department of Health and Human Services Office of Inspector General. “Today we’re sending a strong, clear message to anyone seeking to defraud Medicare: You will get caught and you will pay the price.”
“This case demonstrates the high-level of commitment and perseverance by all law enforcement partners to combat health care fraud,” said Anthony M. DiPaolo, Chief of Investigations for the Insurance Fraud Bureau. “Dr. Mashali took advantage of his patients and deprived them of proper health care while defrauding Medicare and other health care insurers. The IFB has zero tolerance for this type of fraud and continues to fight health care fraud for the citizens of the Commonwealth. The success of this case is due to the collaborative effort of all agencies involved.”
“The sentence imposed by the court today sends a strong message to the health care community – those who defraud Medicare and private insurers to unjustly enrich themselves will pay a hefty price,” said Special Agent in Charge Joel P. Garland, IRS Criminal Investigation. “As a physician entrusted to promote the health of his patients, Mr. Mashali’s conduct is especially egregious. He jeopardized lives by providing substandard care and often prescribed powerful opiates, contributing to the current epidemic. The IRS will continue to bring our financial expertise to health care schemes investigated jointly with our partners.”
-

 Community7 years ago
Community7 years agoNational Shrine of La Salette Festival of Lights 2017 set to begin
-

 Community6 years ago
Community6 years agoMassachusetts State Police looking for good home for retired dogs
-

 Crime6 years ago
Crime6 years agoFall River ranked most dangerous city in Massachusetts according to report
-

 latest7 years ago
latest7 years agoDurfee student allegedly overdoses on marijuana
-

 Community6 years ago
Community6 years agoVideo of Fall River Police goes viral
-

 Causes6 years ago
Causes6 years agoMissing Fall River woman found deceased
-
 Crime6 years ago
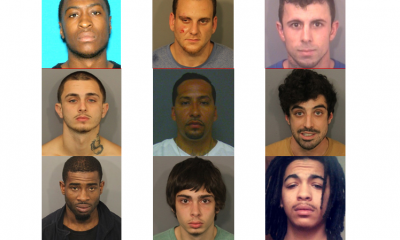
Crime6 years agoFall River Police add names to most wanted list
-

 Causes6 years ago
Causes6 years agoFall River teenager reported missing has been found




