Community
Baker-Polito Administration, Centers for Medicare/Medicaid Services announce $67.2 billion agreement for MassHealth reforms

BOSTON — The Baker-Polito Administration received federal approval today to expand and extend its Medicaid (MassHealth) section 1115 waiver through December 2027. The demonstration approved by the Centers for Medicare and Medicaid Services involves care for MassHealth’s two million members.
“Since Massachusetts implemented its last 1115 Medicaid waiver in 2017, our administration has strengthened and reformed the MassHealth program, focusing on providing a nation-leading health care delivery model that rewards value over volume, and produces better health outcomes for the residents it serves,” said Governor Charlie Baker. “Under this waiver extension, MassHealth will continue to implement innovative reforms that provide quality care, better health outcomes and equity. I am grateful to the Center for Medicare and Medicaid Services for their collaboration with our administration and to Secretary Marylou Sudders, Assistant Secretary Amanda Cassel Kraft and their team for their commitment to improving health care for the people of Massachusetts.”
“Massachusetts’ new 1115 Medicaid waiver will build on our administration’s efforts to ensure the MassHealth system is providing quality, affordable care for the families it services, using an innovative model,” said Lt. Governor Karyn Polito. “The negotiation of this waiver sustains the Commonwealth’s role as a national leader in health care reform and will guide our state’s efforts to strengthen health care deliver for years to come.”
“We’re thrilled to work alongside Massachusetts to advance policies to expand access to high-quality health care, particularly for those most in need,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure. “The demonstration provides 24 months of continuous Medicaid coverage to communities who are among the most likely to experience gaps in coverage – such as those experiencing homelessness. The demonstration also invests in the services that people need to address their health-related social needs, such as medically tailored meals and housing supports. That’s transformational change – as are many of the other components included in Massachusetts’ 1115 demonstration. We encourage all states to follow the Commonwealth’s lead supporting whole-person coverage and care.”
Under the previous 1115 demonstration (2017-2022), the Baker-Polito Administration implemented the significant reforms to the MassHealth program, restructuring the health care delivery system towards integrated, value-based care, including establishing a model of Accountable Care Organizations that now cover over 80% of eligible MassHealth members. The agreement signed today extends and expands key initiatives including ACOs, the Community Partners program that provides wrap-around behavioral health and long-term services and supports for high-risk members, the Flexible Services program that provides nutrition and housing supports, and expanded behavioral health services. The agreement also authorizes new initiatives, including $400 million in annual investments in health equity and a value-based payment program for primary care.
“This 1115 demonstration reinforces Massachusetts’ commitment to providing high quality care for all residents, including individuals and families served by MassHealth,” said Marylou Sudders, Secretary of Health and Human Services. “This next phase of the demonstration will make significant investments in behavioral health and primary care, especially for children and adolescents, to further develop a health care delivery system that is patient-focused, equitable and outcomes driven.”
“The 1115 demonstration allows us to deliver health care models focused on accountable, coordinated care that better serve members and prioritize equity,” said Amanda Cassel Kraft, Assistant Secretary for MassHealth. “MassHealth appreciates the support and engagement from both CMS and the Massachusetts health care community. We look forward to continued collaboration with our partners as we implement these important and innovative initiatives.”
MassHealth’s five primary goals for the newly approved 1115 demonstration include:
1) Continue the path of restructuring and re-affirm accountable, value-based care:
-Refine the ACO and Behavioral Health and Long-Term Services and Supports Community Partners programs, increasing expectations while making improvements based on lessons learned.
-Scale successful programs by transitioning ~80% of time-limited Delivery System Reform Incentive Program (DSRIP) funding to ongoing base funding.
2) Reform and invest in primary care, behavioral health, and pediatric care that expands access and moves the delivery system away from siloed, fee-for-service health care:
-Invest $115 million per year in primary care through a value-based sub-capitation payment model that supports team-based, integrated care.
-Support the Commonwealth’s Roadmap for Behavioral Health Reform by expanding behavioral health services, access and integration.
-Invest $43 million over five years in loan repayment and residency training to strengthen and diversify the primary care and behavioral health workforce serving MassHealth members.
-Strengthen expectations for ACOs to invest in pediatric preventive care and coordinate care for children with complex needs.
3) Advance health equity, addressing health-related social needs and specific disparities:
-An over $2 billion initiative over five years to hold ACOs and ACO-participating hospitals accountable for reducing disparities in health care quality and access.
-Implement interventions to address racial and ethnic disparities in maternal health, complementing policies outside of the demonstration including 12-month postpartum eligibility and coverage of doula services.
-Expand the Flexible Services and Community Supports Programs to address health-related social needs such as nutrition and housing, and to provide post-release transition supports for justice-involved members.
4) Sustainably support the Commonwealth’s safety net, including increased funding for safety net providers, with a continued linkage to accountable care:
-Extend and increase Safety Net Provider Payments by $125 million per year and direct the majority of new incentive funding for health equity to safety net hospitals.
-Preserve other long-time funding for the Commonwealth’s safety net (e.g., the Health Safety Net).
-Implement the expanded hospital assessment recently signed into law to fund these important initiatives and other hospital programs (e.g., increased base rates and a revamped clinical quality program).
5) Maintain near-universal health insurance coverage
-Maintain current coverage expansions, including state subsidies to ensure affordability of Health Connector plans for enrollees with incomes up to 300% of the federal poverty level.
-Make targeted updates to MassHealth eligibility to support coverage and equity, including:
o A simplified process for adults with disabilities to qualify for CommonHealth;
o 3-month retroactive eligibility for pregnant individuals and children;
o At least 12 months of continuous eligibility for members experiencing homelessness and members recently released from a correctional institution; and
o Expanded access to Medicare Savings Programs for members with MassHealth Standard.
-

 Community7 years ago
Community7 years agoNational Shrine of La Salette Festival of Lights 2017 set to begin
-

 Community6 years ago
Community6 years agoMassachusetts State Police looking for good home for retired dogs
-

 Crime6 years ago
Crime6 years agoFall River ranked most dangerous city in Massachusetts according to report
-

 latest7 years ago
latest7 years agoDurfee student allegedly overdoses on marijuana
-

 Community6 years ago
Community6 years agoVideo of Fall River Police goes viral
-

 Causes6 years ago
Causes6 years agoMissing Fall River woman found deceased
-
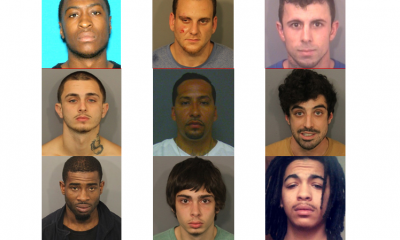
 Crime6 years ago
Crime6 years agoFall River Police add names to most wanted list
-

 Causes6 years ago
Causes6 years agoFall River teenager reported missing has been found




