latest
Audit finds that fed program was paid with state taxpayer money concerning MassHealth

BOSTON – In an audit released today by the Office of State Auditor Suzanne M. Bump, MassHealth agreed to improve its systems for avoiding costs for hospice services that should instead be paid for by the federal government’s Medicare program. The audit examined the period January 1, 2015 through July 31, 2019 and was performed in collaboration with the U.S. Department of Health and Human Services Office of Inspector General’s Boston office, which concurred with the State Auditor’s findings.
The audit found that, because MassHealth was not requiring hospice service providers to notify the agency when it began providing services to MassHealth members or requiring ongoing collaboration of services to these so-called dual-eligible persons, the Commonwealth improperly paid for some services, durable medical equipment and transportation costs, and was at great risk of significant improper payments. During the audit period, MassHealth spent $620 million on hospice-related services provided to 38,568 dual-eligible members.
“This audit, which was performed at the suggestion of and in partnership with the U.S. HHS Inspector General’s Office, provides critical insight relative to the elements of proper claims payments for care for certain persons at the end of life. MassHealth’s deficiencies in checking dual-eligible member claims have resulted in improper state spending for hospice services. We applaud MassHealth’s acceptance of our recommendations to correct these deficiencies,” Bump said. “This audit will not only benefit MassHealth and the state’s taxpayers, but also Massachusetts hospice providers and the federal offices of Health and Human Services and the Centers for Medicare and Medicaid Services, who may now enter similar collaborations with other state auditors.”
Under federal regulations, hospice providers must direct, coordinate, and supervise all services for dual-eligible members receiving hospice care. The audit found MassHealth may have paid an estimated $45,110,697 in claims for services, such as home health aide, homemaker services, and companion care that were not coordinated by members’ hospice providers. Instead, these services were arranged by members, their relatives, or others without the hospice providers’ knowledge, resulting in MassHealth being billed directly.
The audit recommends MassHealth work with the Centers for Medicare & Medicaid Services (CMS) and each of its hospice providers to better obtain hospice information about dual-eligible members and determine whether all required patient forms for hospice care have been submitted. The audit also calls on MassHealth to improve its claim-checking system to ensure it can detect and deny improper claims and costs. Based on its response during the audit process, MassHealth has taken steps to address these recommendations.
Further, in examining the agency’s oversight of hospice providers, the audit found MassHealth does not require providers to submit any plans of hospice care. At least three other states’ Medicaid departments, including Nebraska, Nevada, and West Virginia, have such a requirement in place. The audit notes that if MassHealth were to begin requiring the submission of plans of care from providers, it could limit the risk of improper payments. Lastly, the audit suggests that the agency consider providing additional guidance to hospice providers on expenses that can be billed to MassHealth.
According to the CMS, the Fiscal Year 2020 national Medicaid improper payment rate estimate is approximately 21%, representing over $86 billion in improper payments. The OSA’s collaboration with the HHS Office of Inspector General’s Boston office is a critical partnership that allows for joint reviews of rising Medicaid costs. The audit will be the subject of a joint presentation by the OSA and the HHS OIG this week at a national virtual conference sponsored by the Association of Government Accountants. The last audit conducted collaboratively with the HHS Office of Inspector General’s Boston office was in October 2008, when an audit was conducted of Medicaid claims for personal care attendant services provided to beneficiaries during inpatient stays.
MassHealth provides access to healthcare services for approximately 1.8 million eligible low- and moderate-income children, families, seniors, and people with disabilities annually. In fiscal year 2019, MassHealth paid healthcare providers more than $16 billion, of which approximately 50% was funded by the Commonwealth. Medicaid expenditures represent approximately 39% of the Commonwealth’s total annual budget.
-

 Community6 years ago
Community6 years agoNational Shrine of La Salette Festival of Lights 2017 set to begin
-

 Community6 years ago
Community6 years agoMassachusetts State Police looking for good home for retired dogs
-

 Crime6 years ago
Crime6 years agoFall River ranked most dangerous city in Massachusetts according to report
-

 latest6 years ago
latest6 years agoDurfee student allegedly overdoses on marijuana
-

 Community6 years ago
Community6 years agoVideo of Fall River Police goes viral
-

 Causes6 years ago
Causes6 years agoMissing Fall River woman found deceased
-
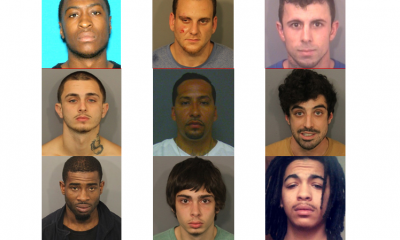
 Crime6 years ago
Crime6 years agoFall River Police add names to most wanted list
-

 Causes6 years ago
Causes6 years agoFall River teenager reported missing has been found




