latest
Biden-Harris Administration to require insurance, group health plans to cover cost of at-home COVID-19 tests
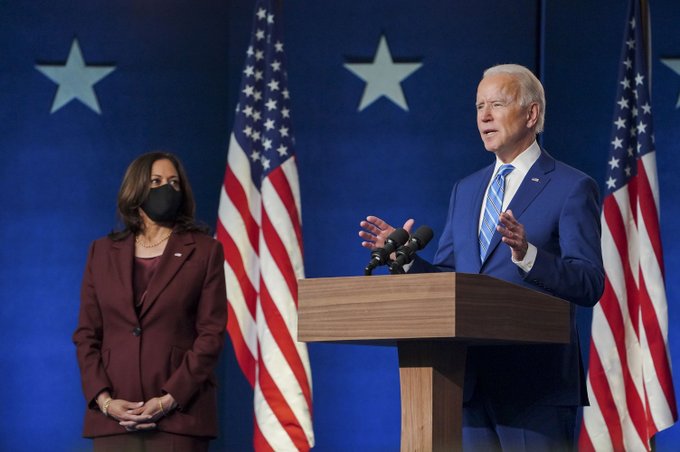
The Biden-Harris Administration is requiring insurance companies and group health plans to cover the cost of over-the-counter, at-home COVID-19 tests, so people with private health coverage can get them for free starting January 15th. The new coverage requirement means that most consumers with private health coverage can go online or to a pharmacy or store, buy a test, and either get it paid for up front by their health plan, or get reimbursed for the cost by submitting a claim to their plan. This requirement incentivizes insurers to cover these costs up front and ensures individuals do not need an order from their health care provider to access these tests for free.
Beginning January 15, 2022, individuals with private health insurance coverage or covered by a group health plan who purchase an over-the-counter COVID-19 diagnostic test authorized, cleared, or approved by the U.S. Food and Drug Administration (FDA) will be able to have those test costs covered by their plan or insurance. Insurance companies and health plans are required to cover 8 free over-the-counter at-home tests per covered individual per month. That means a family of four, all on the same plan, would be able to get up to 32 of these tests covered by their health plan per month. There is no limit on the number of tests, including at-home tests, that are covered if ordered or administered by a health care provider following an individualized clinical assessment, including for those who may need them due to underlying medical conditions.
“Under President Biden’s leadership, we are requiring insurers and group health plans to make tests free for millions of Americans. This is all part of our overall strategy to ramp-up access to easy-to-use, at-home tests at no cost,” said HHS Secretary Xavier Becerra. “Since we took office, we have more than tripled the number of sites where people can get COVID-19 tests for free, and we’re also purchasing half a billion at-home, rapid tests to send for free to Americans who need them. By requiring private health plans to cover people’s at-home tests, we are further expanding Americans’ ability to get tests for free when they need them.”
Over-the-counter test purchases will be covered in the commercial market without the need for a health care provider’s order or individualized clinical assessment, and without any cost-sharing requirements such as deductibles, co-payments or coinsurance, prior authorization, or other medical management requirements.
As part of the requirement, the Administration is incentivizing insurers and group health plans to set up programs that allow people to get the over-the-counter tests directly through preferred pharmacies, retailers or other entities with no out-of-pocket costs. Insurers and plans would cover the costs upfront, eliminating the need for consumers to submit a claim for reimbursement. When plans and insurers make tests available for upfront coverage through preferred pharmacies or retailers, they are still required to reimburse tests purchased by consumers outside of that network, at a rate of up to $12 per individual test (or the cost of the test, if less than $12). For example, if an individual has a plan that offers direct coverage through their preferred pharmacy, but that individual instead purchases tests through an online retailer, the plan is still required to reimburse them up to $12 per individual test. Consumers can find out more information from their plan about how their plan or insurer will cover over-the-counter tests.
“Testing is critically important to help reduce the spread of COVID-19, as well as to quickly diagnose COVID-19 so that it can be effectively treated. Today’s action further removes financial barriers and expands access to COVID-19 tests for millions of people,” said CMS Administrator Chiquita Brooks-LaSure.
State Medicaid and Children’s Health Insurance Program (CHIP) programs are currently required to cover FDA-authorized at-home COVID-19 tests without cost-sharing. In 2021, the Biden-Harris Administration issued guidance explaining that State Medicaid and Children’s Health Insurance Program (CHIP) programs must cover all types of FDA-authorized COVID-19 tests without cost sharing under CMS’s interpretation of the American Rescue Plan Act of 2019 (ARP). Medicare pays for COVID-19 diagnostic tests performed by a laboratory, such as PCR and antigen tests, with no beneficiary cost sharing when the test is ordered by a physician, non-physician practitioner, pharmacist, or other authorized health care professional. People enrolled in a Medicare Advantage plan should check with their plan to see if their plan offers coverage and payment for at-home over-the-counter COVID-19 tests.
The U.S. Department of Health and Human Services (HHS) is also providing up to 50 million free, at-home tests to community health centers and Medicare-certified health clinics for distribution at no cost to patients and community members.







You must be logged in to post a comment Login